3D printed model of arterial valve can help reduce surgical complications
Recently, the University of Washington (UW) in Seattle has successfully developed a method to reduce the risk of complications from transcatheter aortic valve replacement (TAVR) with the help of a 3D printed model of the cardiac aortic valve. For many patients with aortic stenosis, TAVR is a relatively safe treatment because it does not remove the damaged valve but is repaired through the catheter using a collapsible prosthetic valve. Even so, complications can occur with this procedure, the most common of which is valve aortic regurgitation (PAR). It is usually caused by a false installation of the prosthetic valve or a poorly closed circumference. This is mainly because the structure of the aortic root is complicated, the size and shape vary from person to person, so it is difficult for the doctor to determine the size of the prosthetic valve. . But now, with the 3D printed valve method developed by UW, everything will be solved, because the biggest advantage of 3D printing is the ability to accurately personalize.
It is understood that the main principle of UW this method is to use the 3D printing model of the valve to help the doctor accurately assess the effect of the valve. To test the feasibility of this method, the research team invited 16 patients who had undergone TAVR to conduct an experiment. Eight of them had experienced PAR, and the other eight had not experienced it, but for comparison, the age, gender, and size of the implanted valve were similar to those of the first nine. In the experiment, the team first acquired the heart valve data of all patients, and then made the corresponding solid model using SLA and FDM 3D printers respectively, except that the former was soft and the latter was relatively hard. In order to ensure the accuracy of the model, they also compared the measurement with the CT scan image.
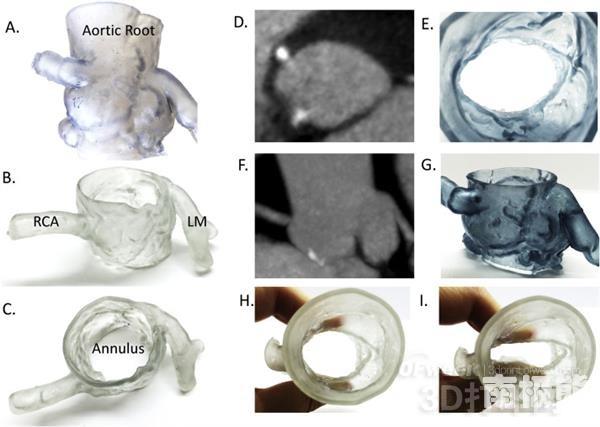
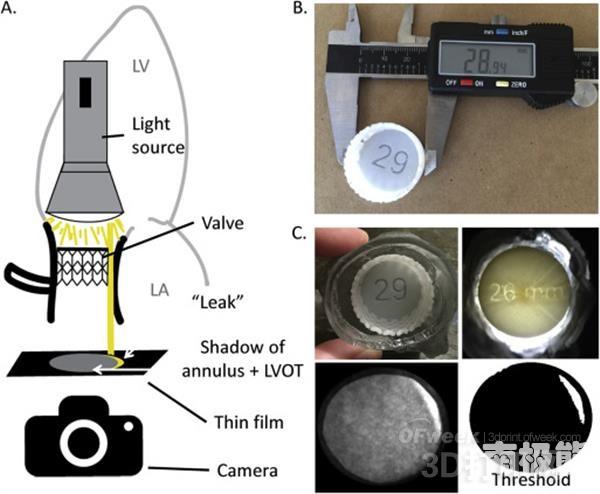
After the model was done, the researchers used a clever method to assess the likelihood of PAR: they applied a valve model printed for PAR patients to the real valve that these people had implanted, and then used a A simple photographic technique is used to detect the amount of light that passes through the left ventricular outflow tract. (That means to determine if the valve is completely sealed), they did the same for the control group that had not experienced PAR. As a result, this photodetection method successfully identified 6 out of 9 PAR patients (up to 66% success rate) and successfully excluded 5 of 7 patients who had not experienced PAR (up to 71% success rate). The change here is because one of the latter is considered to be more likely to have PAR in the future. Although the accuracy rate is not 100%, the researchers believe that this method is still feasible. In the future, as long as you use this method to determine the potential risk of PAR, you can choose not to use TAVR, but choose other treatment methods. Currently, researchers have written the study into a paper published in the journal Cardiovascular Computed Tomography.
Serving Spoon,Salad Spoons,Gold Serving Utensils,Serving Spoon Sets
Taizhou Polybest Household Product Co.,Ltd , https://www.polycutlery.com